Research with exotic viruses risks a deadly outbreak, scientists warn
A growing number of scientists are reconsidering the dangers of prospecting for unknown viruses and conducting other high-stakes work with pathogens

BANGKOK — When the U.S. government was looking for help to scour Southeast Asia’s rainforests for exotic viruses, scientists from Thailand’s Chulalongkorn University accepted the assignment and the funding that came with it, giving little thought to the risks.
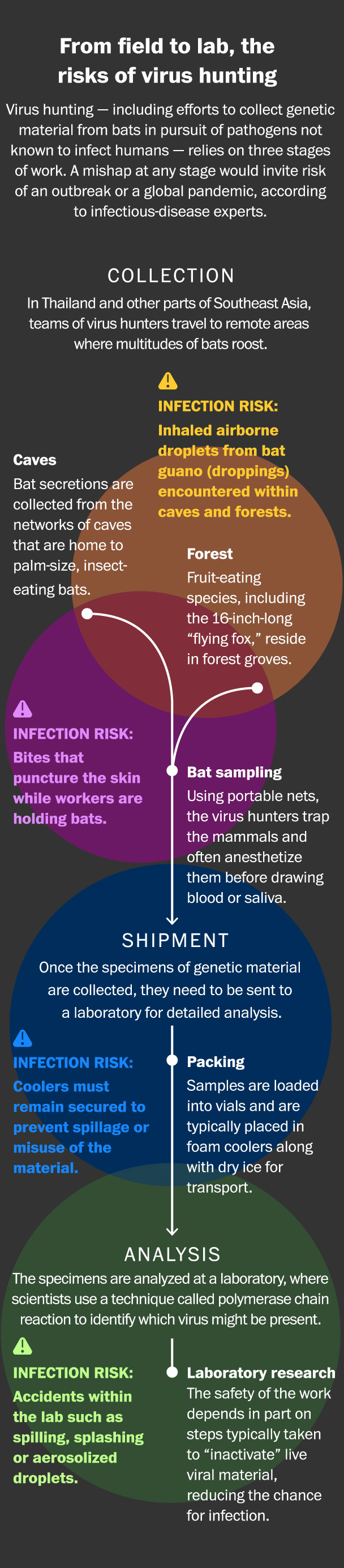
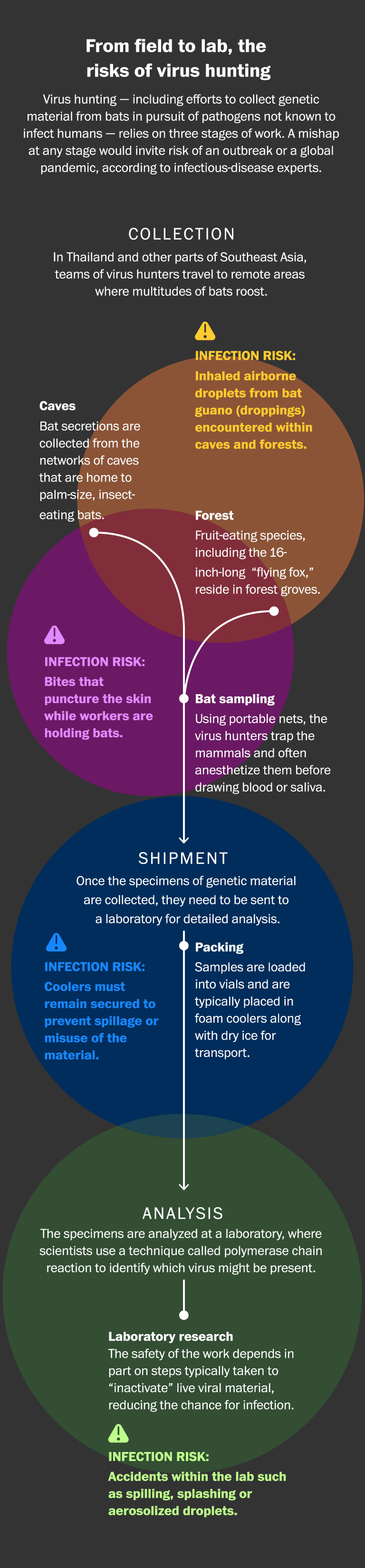
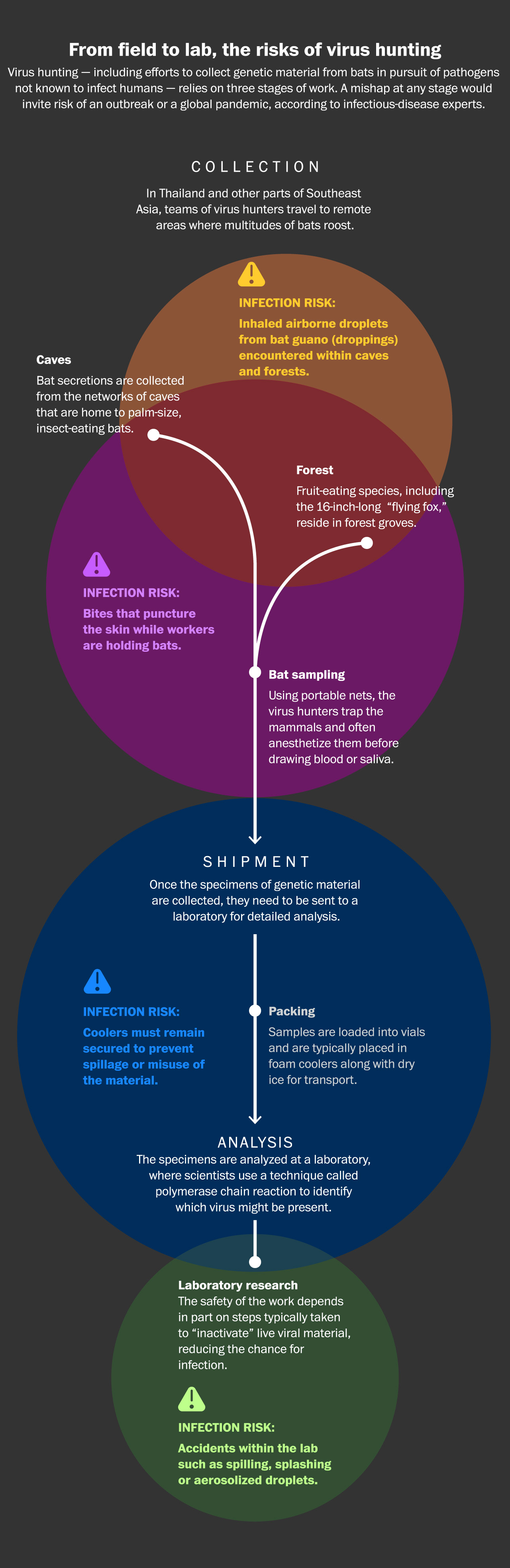
Beginning in 2011, Thai researchers made repeated treks every year to remote caves and forests inhabited by millions of bats, including species known to carry diseases deadly to humans. The scientists collected saliva, blood and excrement from the wriggling, razor-fanged animals, and the specimens were placed in foam coolers and driven to one of the university’s labs in Bangkok, a metropolis of more than 8 million people.
The goal was to identify unknown viruses that might someday threaten humans. But doubts about the safety of the research began to simmer after the virus hunters were repeatedly bitten by bats and, in 2016, when another worker stuck herself with a needle while trying to extract blood from an animal.
Some of the workers received booster shots to prevent infection by common rabies, and none of them reported illness, according to their supervisor. But the incidents raised disturbing questions about the research: What if they encountered an unknown virus that killed humans? What if it spread to their colleagues? What if it infected their families and neighbors?
As if to underscore the risks, in 2018 another lab on the same Bangkok campus — a workspace built specifically to handle dangerous pathogens — was shut down for months because of mechanical failures, including a breakdown in a ventilation system that guards against leaks of airborne microbes. Then, in a catastrophe that began in Wuhan, a Chinese city 1,500 miles away, the coronavirus pandemic swept the globe, becoming a terrifying case study in how a single virus of uncertain origin can spread exponentially.
In spring 2021, the Thai team’s leader pulled the plug, deciding that the millions of dollars of U.S. research money for virus hunting did not justify the risk.
“To go on with this mission is very dangerous,” Thiravat Hemachudha, a university neurologist who supervised the expeditions, told The Washington Post. “Everyone should realize that this is hard to control, and the consequences are so big, globally.”
Three years after the start of the coronavirus pandemic, a similar reckoning is underway among a growing number of scientists, biosecurity experts and policymakers. The global struggle with covid-19, caused by the novel coronavirus, has challenged conventional thinking about biosafety and risks, casting a critical light on widely accepted practices such as prospecting for unknown viruses.
A Post examination found that a two-decade, global expansion of risky research has outpaced measures to ensure the safety of the work and that the exact number of biocontainment labs handling dangerous pathogens worldwide, while unknown, is believed by experts to be in the thousands.
In scores of interviews, scientific experts and officials — including in the Biden administration — acknowledged flaws in monitoring the riskiest kinds of pathogen research. While the pandemic showcased the need for science to respond quickly to global crises, it also exposed major gaps in how high-stakes research is regulated, according to the interviews and a review of thousands of pages of biosafety documents. The source of the coronavirus pandemic remains uncertain. While many scientists and experts suspect it may have been caused by a natural spillover from animals to humans, the FBI, including Director Christopher A. Wray, and a recent Energy Department assessment concluded with varying degrees of confidence that its likely source was an accidental release from a lab in Wuhan.
Within the United States, government regulation has also failed to keep step with new technologies that allow scientists to alter viruses and even synthesize new ones. The Biden administration is expected this year to impose tighter restrictions on research with the kinds of pathogens that could trigger an outbreak or a pandemic, according to officials familiar with the matter who spoke on the condition of anonymity to discuss internal deliberations.
Governments and private researchers continue building high-containment laboratories to work with the most menacing pathogens, despite a lack of safety standards or regulatory authorities in some countries, science and policy experts said. Meanwhile, U.S. agencies continue to funnel millions of dollars annually into overseas research, such as virus hunting, that some scientists say exposes local populations to risks while offering few tangible benefits.
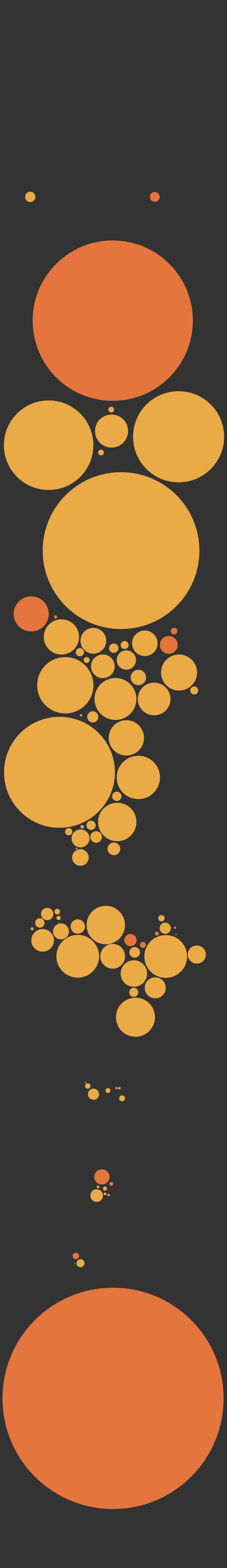
Spending by the United States
on pathogen research
worldwide
Since 2012, the United States has spent
billions of dollars to combat, prevent and
surveil zoonotic viruses and other
infectious microbes globally. The federal
government has devoted nearly
$3 billion to work and research related to
zoonotic pathogens in at least 78 countries
and more than 10 regions around the world.
Country or territory
Region
Regional funding
consists of programs
and activities that
span multiple
countries
Africa
West Africa
$448M
Sierra Leone
Senegal
$144M
Guinea
$139M
Liberia
$429M
Sub-Saharan
Africa
Mali
Burkina
Faso
Eastern
Africa
Egypt
Nigeria
Ghana
Ethiopia
Sudan
Ivory Coast
$55M
South
Sudan
Somalia
Cameroon
Kenya
Democratic
Republic
of the Congo
Uganda
$214M
Tanzania
Zimbabwe
Madagascar
South Africa
Asia
Armenia
Georgia
Jordan
Bangladesh
China
$25M
Israel
Pakistan
$2M
Asia
Vietnam
India
Myanmar
$31M
Yemen
$31M
Philippines
Thailand
Malaysia
Cambodia
Indonesia
$26M
North America
Mexico
Jamaica
Barbados
Guatemala
$2M
South America
Latin America and
Caribbean
Ecuador
Brazil
Peru
$2M
Europe
Europe and Eurasia
Ukraine
$537,000
Global programs
$854M
Note: Excludes Russia, Turkey and Azerbaijan. Money
allocated for work in these countries was canceled or
readjusted because of changes in scope of the projects
and activities.
Source: ForeignAssistance.gov
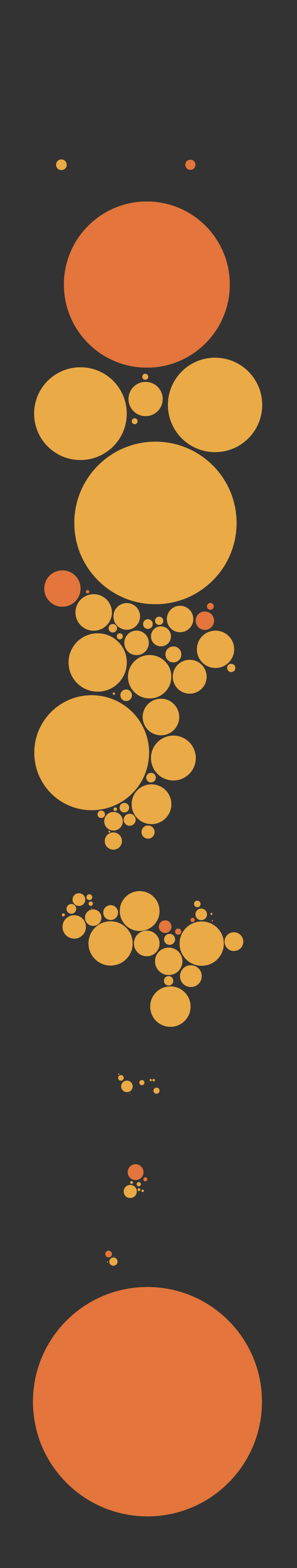
Spending by the United States on
pathogen research worldwide
Since 2012, the United States has spent billions of
dollars to combat, prevent and surveil zoonotic
viruses and other infectious microbes globally.
The federal government has devoted nearly
$3 billion to work and research related to zoonotic
pathogens in at least 78 countries and more than
10 regions around the world.
Country or territory
Region
Africa
Regional funding
consists of
programs and
activities that
span multiple
countries
West Africa
$448M
Sierra Leone
Senegal
$144M
Guinea
$139M
Liberia
$429M
Sub-Saharan
Africa
Mali
Burkina
Faso
Egypt
Eastern Africa
Nigeria
Ghana
Ethiopia
Sudan
Ivory Coast
$55M
South
Sudan
Somalia
Cameroon
Kenya
Democratic
Republic
of the Congo
Uganda
$214M
Tanzania
Zimbabwe
Madagascar
South Africa
Asia
Georgia
Armenia
Bangladesh
Jordan
China
$25M
Israel
Pakistan
$2M
Asia
India
Myanmar
Vietnam
Yemen
$31M
$31M
Philippines
Thailand
Malaysia
Cambodia
Indonesia
$26M
North America
Mexico
Jamaica
Barbados
Guatemala
$2M
South America
Latin America and
Caribbean
Ecuador
Brazil
Peru
$2M
Europe
Europe and Eurasia
Ukraine
$537,000
Global programs
$854M
Note: Excludes Russia, Turkey and Azerbaijan. Money allocated for work
in these countries was canceled or readjusted because of changes in
scope of the projects and activities.
Source: ForeignAssistance.gov
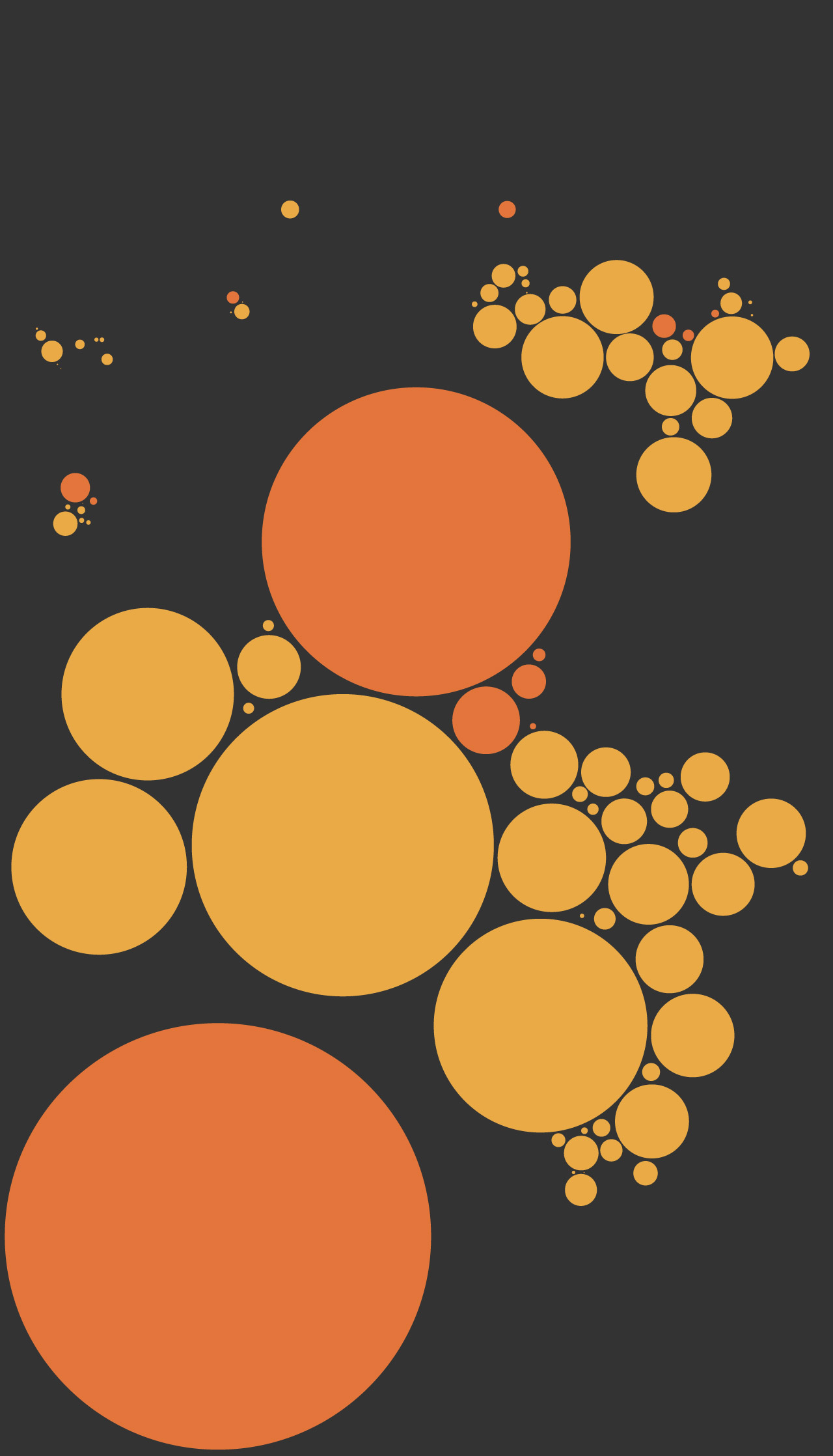
Spending by the United States on
pathogen research worldwide
Since 2012, the United States has spent billions of dollars to combat, prevent and surveil
zoonotic viruses and other infectious microbes globally. The federal government
has devoted nearly $3 billion to work and research related to zoonotic pathogens
in at least 78 countries and more than 10 regions around the world.
Country or territory
Region
Georgia
North
America
Europe
Armenia
Asia
Mongolia
Bangladesh
Europe and Eurasia
Jordan
China
$25M
Pakistan
Asia
Ukraine
$2M
Yemen
Mexico
$537,000
Vietnam
Myanmar
$31M
India
Barbados
Guatemala
$31M
Philippines
$2M
Thailand
South
America
Malaysia
Cambodia
Indonesia
Latin America and
Caribbean
$26M
West Africa
Peru
$448M
$2M
Regional funding consists
of programs and
activities that span
multiple countries
Africa
Senegal
Eastern Africa
Guinea
Sub-Saharan
Africa
$139M
Mali
Burkina
Faso
Egypt
Nigeria
Ghana
Ethiopia
Liberia
Sudan
Ivory Coast
$429M
Sierra Leone
$55M
$144M
South
Sudan
Cameroon
Kenya
Democratic
Republic
of the Congo
Uganda
$214M
Tanzania
Zimbabwe
Madagascar
South Africa
Global programs
$854M
Note: Excludes Russia, Turkey and Azerbaijan.
Money allocated for work in these countries
was canceled or readjusted because of
changes in scope of the projects and activities.
Source: ForeignAssistance.gov
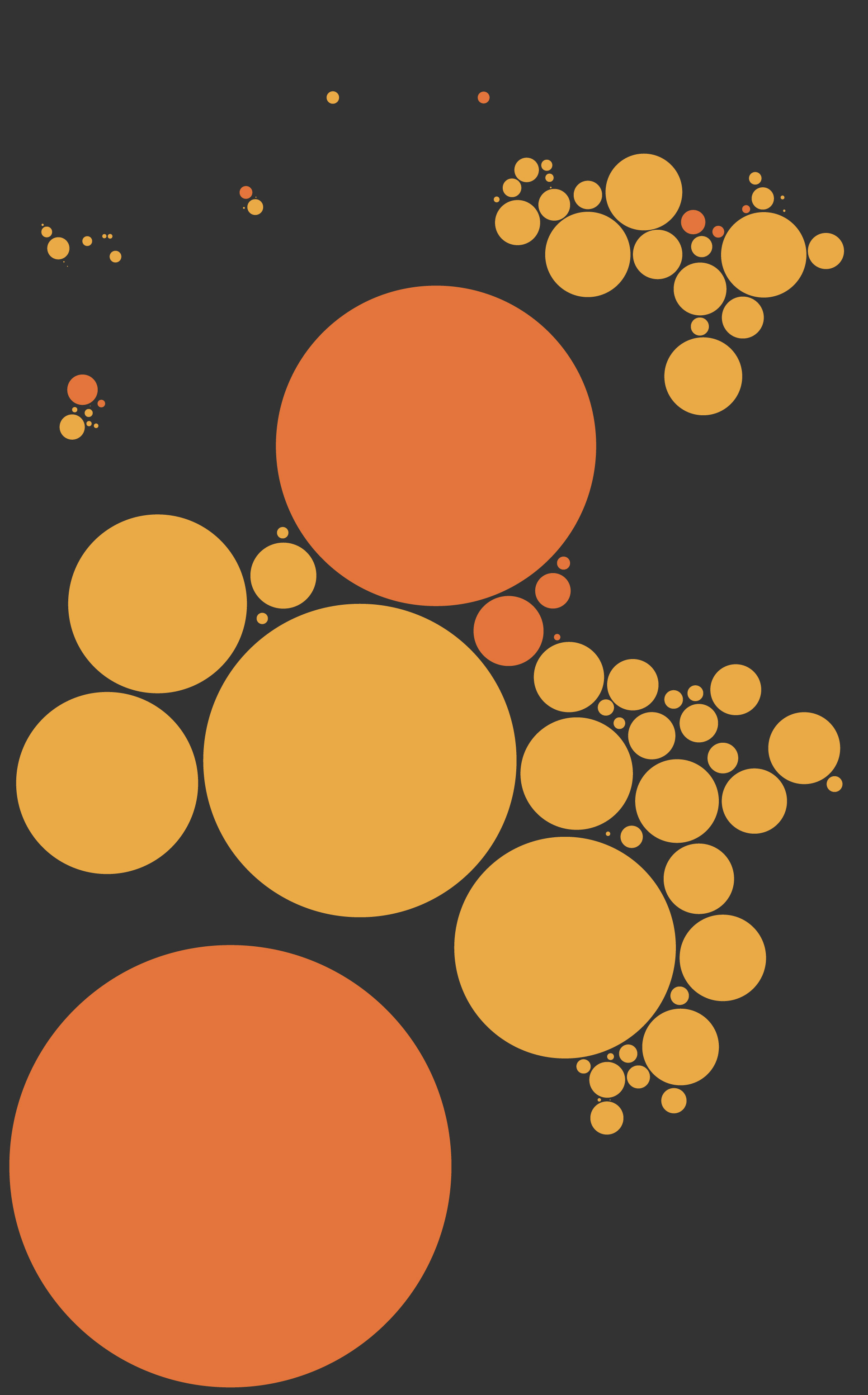
Spending by the United States on pathogen research worldwide
Since 2012, the United States has spent billions of dollars to combat, prevent and surveil zoonotic viruses and other infectious
microbes globally. The federal government has devoted nearly $3 billion to work and research related to
pathogens spreadable between people and animals in at least 78 countries and more than 10 regions around the world.
Country or territory
Region
Georgia
North
America
Armenia
Europe
Asia
Mongolia
Jordan
Bangladesh
Europe and Eurasia
Nepal
China
$25M
Israel
Pakistan
$2M
Ukraine
Asia
Yemen
$537,000
Mexico
Jamaica
Laos
India
Vietnam
Myanmar
Barbados
$31M
$31M
Guatemala
Philippines
$2M
Thailand
South
America
Cambodia
Malaysia
Indonesia
Latin America and
Caribbean
$26M
Ecuador
Brazil
West Africa
Regional funding consists
of programs and
activities that span
multiple countries
Peru
$448M
$2M
Africa
Senegal
Eastern Africa
Guinea
$139M
Sub-Saharan
Africa
Mali
Burkina
Faso
Egypt
Nigeria
Ghana
Ethiopia
Liberia
Sudan
Ivory Coast
$429M
Sierra Leone
$55M
$144M
South
Sudan
Somalia
Cameroon
Kenya
Democratic
Republic
of the Congo
Uganda
$214M
Tanzania
Zimbabwe
Madagascar
South Africa
Global programs
$854M
Note: Excludes Russia, Turkey and Azerbaijan. Money allocated for work in
these countries was canceled or readjusted because of changes in scope
of the projects and activities.
Source: ForeignAssistance.gov
“If you stand back and look at the big picture, the science is rapidly outpacing the policy and the guardrails,’’ said James Le Duc, an infectious-disease expert who led research for the U.S. Army and the Centers for Disease Control and Prevention before directing a maximum-containment lab complex at the University of Texas at Galveston.
“This is a national security concern,” he said. “It’s a global public health concern.”
Hunting for trouble
A few hours’ drive outside Bangkok are lush rainforests and craggy highlands that are home to dense swarms of bats — ranging from palm-sized insect eaters to foot-long species that feast on fruit. Thai researchers had long monitored the bats for deadly strains of viruses known to infect humans, including rabies and severe acute respiratory syndrome, called SARS.
But the virus hunting performed there over the past decade at U.S. government expense included a different goal — to discover pathogens unknown to science.
Chulalongkorn University, Thailand’s oldest and one of Southeast Asia’s top-ranked biomedical institutions, became a hub for U.S.-funded projects that called for the collection and study of viruses on a vastly larger scale. Rather than focusing on pathogens that had made the jump to humans, the goal was to find and genetically evaluate viruses still circulating principally among animals, project documents show. By building extensive databases of these viruses, U.S. sponsors of the research — including the Pentagon’s Defense Threat Reduction Agency and the U.S. Agency for International Development — hoped to forecast which of the microbes might threaten humans.
Thiravat, the physician who oversaw the work with wildlife pathogens, recalled that he initially welcomed the chance in 2011 to partner with American scientists in the Pentagon-funded virus-hunting program called Prophecy. The following year, the visitors from the United States were touting a similar project, called PREDICT, with an overall $200 million budget administered by USAID. The goal was to identify pathogens “most likely to become pandemic” and prevent such events.
The virus hunting typically started with flights or difficult drives to remote provinces where clusters of trees and networks of caverns provided sanctuary for bat colonies. The Thai researchers would approach the caves and roosting trees at dusk, just as the nocturnal inhabitants were beginning to stir, and work until dawn, catching some in nets and grasping them with gloved hands so that the bodily fluids could be collected on swabs for analysis.
Sometimes, Thiravat removed his cumbersome rubber gloves to make the task easier.
“In the early days, we didn’t think it was that harmful,” he said.
Humans can become infected through direct contact with the bats’ secretions, including their droppings, which are mined as fertilizer in parts of Southeast Asia. “We were really lucky,” Thiravat said, that no one died.
Over time, Thiravat said he grew worried about the risk of accidental infection — in the field, and as the vials of bat material were transported back to his campus lab in Bangkok — where workers clad in protective masks and coats genetically sequenced the viruses using a technique called polymerase chain reaction. Before those analyses began on the lab’s cramped ninth floor, technicians in the field sought to “inactivate” the specimens to prevent the viral material from infecting anyone.
For more than a decade, the process of collection, transportation and analysis played out several times a year. One misstep could invite trouble: a virus-contaminated needle piercing latex and skin in the field, a spill in transit or an equipment malfunction in the lab.
In China, where a separate virus-cataloguing effort has been underway for years, scientists have described being bitten or scratched by bats or having bat urine or blood splashed into their eyes and faces. A 25-year-old American researcher became ill with a Sosuga virus in 2012 after a research expedition to Sudan and Uganda to collect blood and tissue from bats and rodents. She survived after being hospitalized for 14 days upon returning to the United States, suffering from fever, malaise, headache and muscle and joint pain, according to CDC scientists. The virus, rarely detected in humans, is endemic among the African region’s jumbo-sized fruit bats.
In 2018, at Chulalongkorn, the scientists were shaken when technicians discovered malfunctioning safety equipment at another lab operating on the same floor as the one used by the virus hunters, according to Thiravat. The technicians found a fault in an air-pressure system designed to keep dangerous microbes from infecting lab workers, and a broken autoclave, a high-pressure steam sterilizer necessary to inactivate and safely dispose of viruses or other contaminated materials. No sicknesses were reported.
Repairs were ordered, and the lab was shut down for six months, Thiravat and two colleagues who help operate the facility, Chanida Ruchisrisarod and Teerada Ponpinit, told The Post. The deficiencies have not previously been publicized.
In early 2021, with Thailand’s death toll in the coronavirus pandemic topping 22,000, Thiravat began informing his U.S. contacts and others that he was finished with virus hunting. A decade of work, he said, had produced no discernible benefit for Thailand while exposing his researchers to life-threatening risk. Thiravat told American officials that the U.S. money — about $10 million of it had flowed to his team’s operations — would be better spent on mosquito nets and other conventional public health measures proven to save lives. The field workers’ earlier bat bites also weighed on him.
In an email to a Pentagon grants official and others, he described a “paradigm shift” in his decision to move away from virus hunting.
“Instead of wildlife surveillance that revealed hundreds of viruses belonging to many families — including coronaviruses that may or may not jump to humans,’’ Thiravat wrote on April 14, 2022, “we focus on attempting to identify what is responsible for illness in humans and animals.” A copy of the correspondence was obtained by The Post.
The associate dean for research at Chulalongkorn, Vorasuk Shotelersuk, acknowledged Thiravat’s decision while saying that university policy does not prohibit collecting wildlife viruses. “I see that it has some risks,” Vorasuk said. “But I see that it’s possible that … the risks can be handled properly.”
A spokeswoman for the Pentagon’s Defense Threat Reduction Agency, Andrea Chaney, said it now funds “no active bio-surveillance studies in Thailand” but “would be eager to partner with Thailand on future projects.”
On Friday, Thiravat said he had ordered destruction of the thousands of bat specimens collected during virus hunting expeditions and stored at the university.
Explosive growth
Until the early 21st century, research into the most lethal pathogens — including the Ebola and Marburg viruses — was typically the domain of a handful of fortresslike laboratories around the world, such as those at Fort Detrick, Md., where scientists performed their tasks with elaborate protective gear, including air-purifying respirators and full-body pressurized suits.
But the 2001 American anthrax-letter attacks and later outbreaks of biological threats such as Ebola sparked a construction boom. Funded in part by millions of U.S. dollars, governments worldwide built additional maximum containment labs, which some officials promoted as bulwarks against bioterrorism that would also help diagnose newly emerged human infections, and speed research that could deliver lifesaving vaccines or therapeutics.
The number of labs continues to soar. Of the most restrictive, known as Biosafety Level (BSL) 4 labs, some 69 exist or are under construction in 27 countries. Half were built in the past decade, including 10 last year, according to data gathered for a newly released report by Global Biolabs, a British-U.S. consortium that advocates for vigorous oversight of pathogen research.

Podcast episode
The virus hunters
The growth in research also has driven construction of a slightly less-restrictive type of laboratory, known as the BSL-3. These labs are designed to handle sometimes-fatal pathogens such as plague and anthrax and the viruses that cause covid-19 and West Nile fever. The Bangkok laboratory that was shut down over safety concerns in 2018 is rated BSL-3.
Although no reliable totals exist for the number of BSL-3 labs globally — scientists suspect there are perhaps thousands — the federal Government Accountability Office has listed 1,362 in the United States alone, most of those operated by the federal government, state governments or academic institutions.
But the GAO noted that its number is an incomplete count. “We found that there are entities that have high-containment labs but have not registered” with the federal government, Kelly L. DeMots, a GAO assistant director for health care, told The Post. Labs are required to register if they are working with dangerous microbes, including Ebola, anthrax and more than 60 other pathogens and toxins.
The CDC inspects the registered labs, which are supposed to disclose accidents or mishaps. From 2009 to 2018, such labs reported an average of 98 incidents annually, ranging from minor problems with protective gear to exposures from accidental jabs with contaminated needles, according to CDC records.
A separate accounting, based on National Institutes of Health records obtained by private researchers through the Freedom of Information Act, identified 184 incidents between 2004 and 2018. They all occurred in labs rated at BSL-2 or higher and included spills of contaminated wastes, bites from infected animals and label mix-ups that resulted in workers unknowingly handling live viruses, according to an analysis by Lynn Klotz, a senior science fellow at the Center for Arms Control and Non-Proliferation in D.C.
The BSL-2 labs handle infectious pathogens or toxins that pose a moderate risk if inhaled, swallowed or exposed to the skin. Labs designated BSL-1 should have some personal protective equipment and an autoclave for decontaminating materials.
Several lab workers identified in NIH records tested positive for exposure to dangerous pathogens, Klotz’s research showed, although there were no reports of serious illnesses or exposures to people outside the labs, according to his analysis, which he provided to The Post.
A GAO report released in January revealed multiple gaps in the federal government’s policing of the riskiest kinds of experiments. The report, which identified no labs by name, said the Department of Health and Human Services is providing “subjective and potentially inconsistent” oversight of U.S.-funded research. Additionally, “HHS does not conduct oversight” of research funded by foundations and other nongovernment groups, even when the work involves “enhancement of potential pandemic pathogens.”
Far less is known about labs outside the United States. Regulation falls to each individual country, and there are no enforced international standards.
Global Biolabs, the advocacy group, found that nearly 1 in 10 BSL-4 labs operating in other countries score poorly in international rankings for lab safety. In some cases, labs were constructed without local regulations or meaningful oversight of the handling of dangerous pathogens, or “even a well-established culture of responsible research,” said Gregory Koblentz, a co-author of the Global Biolabs report and the director of the biodefense graduate program at George Mason University’s Schar School of Policy and Government.
Most countries lack the sophisticated controls needed to prevent dangerous viruses or bacteria from being misused or diverted for illicit purposes, he said. “This is a major blind spot in global surveillance for future biological threats,” Koblentz said.
Neither are there reliable sources of information on research accidents, especially in developing countries, where laboratories often struggle to pay the bills and sometimes are forced to contend with blackouts and shortages of clean water, according to interviews with scientists and other experts.
“In some parts of the world, they just don’t have the people, the money or the need” for the research performed at the high containment labs, said Thomas Inglesby, a biosecurity adviser to multiple U.S. administrations who also is the director of the Johns Hopkins Center for Health Security in Baltimore.
Scientists and officials contacted in Southeast Asia and Africa, for instance, described constant struggles to fund salaries and the training of lab personnel, along with paying for protective gear, replacement parts and other upkeep of safety systems. “My worry is the maintenance and the costs,” Oyewale Tomori, a virologist and former president of the Nigerian Academy of Science, said in an interview from Lagos. Tomori is “very concerned” with the several BSL-3 labs operating in Nigeria, he said, “because the funding to maintain and sustain” biosafety is lacking.
At the World Health Organization, epidemiologist Kazunobu Kojima has for more than a decade led its efforts to encourage countries to reduce the risks, revising, for example, a biosafety manual that labs are encouraged to adopt. The WHO, Kojima said by email, has found that poorer countries — which he declined to name — “struggle to attain the necessary capacities and capabilities to manage biosafety and biosecurity challenges.”
The U.S. National Academy of Sciences also has sought for more than a decade to promote safety by inviting international lab specialists to conferences and asking them privately to share their concerns. Interviews with participants and conference summaries reviewed by The Post reveal long-standing deficiencies.
“Major gaps in biosafety implementation’’ were reported in the Caribbean region, “where a survey of 13 major labs found that only about half the respondents indicated that respirators were used correctly,” according to the summary of a conference held in 2011 in Istanbul.
Of about 45 BSL-3 facilities operating in Southeast Asia, “questions exist about standards, management, training and security for most labs in the region,’’ according to the summary. Many lab safety cabinets — intended to contain pathogenic material aerosolized during experiments — were “neither functional nor regularly inspected,’’ according to a second account of the meeting prepared by the National Academy of Sciences, which added: “For some labs, the availability of electricity and water was severely limited.”
In 2016, scientists who gathered again warned of systemic lab deficiencies in Asia.
In Malaysia, “adequate resources are needed to improve basic biosafety infrastructure, facilities and equipment.” In Vietnam, of the country’s more than 5,000 BSL-1 and BSL-2 labs, “only 600 of them are certified” by the government and “most facilities do not yet meet the biosafety conditions.” In India, “awareness about bio-risk management at … many national laboratories is inadequate and … trained staff on biosafety issues is needed.”
Micah Lowenthal, the director of the National Academy’s committee on international security and arms control, said the conferences sought to “reduce the possibility of an outbreak.”
“We want to improve the practices at the laboratories,” said Lowenthal, who is a physicist. The presentations helped demonstrate, he said, “how hard it is to build and run these facilities. They’re expensive; there’s a lot of care that has to go into it.”
Reconsidering the risk
The United States has allocated more than $400 million to virus hunting worldwide since 2009, according to grant documents and other federal records. Proponents contend that this effort could help develop the medicines to counter future spillovers of deadly viruses from animals to humans, and two of the U.S.-funded programs are aimed explicitly at preventing human pandemics.
The Biden administration initially backed the research, announcing on Oct. 5, 2021, a USAID initiative called DEEP VZN (short for “Discovery & Exploration of Emerging Pathogens — Viral Zoonoses”) in Africa, Asia and Latin America. The program would “detect, prevent and respond to future biological threats,” USAID said at the time.
“DEEP VZN will build and expand on previous work by significantly scaling up USAID’s efforts to understand where, when, and how viruses spillover from animals to humans,’’ said an agency news release, promoting the $125 million program.
But in December 2021, officials with the White House National Security Council and the Office of Science and Technology Policy privately advocated to end DEEP VZN and another USAID program called “STOP Spillover,” a $100 million effort to analyze disease threats from animals and prevent outbreaks or pandemics.
According to interviews with people familiar with the matter, who spoke on the condition of anonymity to discuss internal administration deliberations, the officials made their recommendation personally and in emails to USAID Administrator Samantha Power and her top aides. Power pledged a review of the research programs, which continue to receive USAID funding. During the review, the agency has directed field researchers to delay their collection of viral samples until officials can ascertain that sufficient steps have been taken to ensure the safety of the work, agency officials said. A USAID spokeswoman told The Post the field work would remain suspended while the agency “ensures rigorous safeguards are put in place and identified concerns are addressed.”
The White House recommendation was based in part on classified warnings about the possibility that foreign adversaries could use the programs’ data to advance bioweapons programs, said those familiar with the events.
Critics of virus hunting contend that the programs create unacceptable risks and have generated vast amounts of genetic data of limited usefulness. They note that the harvesting of bat viruses failed to predict the coronavirus pandemic or yield new vaccines.
The work provides researchers with a snapshot in time of viruses that are continuously evolving, but “there is no way to know, based on the identification of a virus in an animal, whether it’s going to pose a threat to humans, to livestock or to wildlife,” said W. Ian Lipkin, an epidemiologist at Columbia University. Lipkin said his New York City lab analyzed viruses collected abroad for the U.S. government’s PREDICT program.
Prominent biosecurity specialists also have warned of the appeal to terrorists.
Kevin Esvelt, a Massachusetts Institute of Technology biotechnologist who helped develop the pioneering gene-editing technology known as CRISPR, told members of Congress in December 2021 that posting the genetic sequences of viruses could lead to a global pandemic.
Doing so, he said, is like publicly revealing the instructions for making a nuclear bomb. “If someone were to assemble pandemic-capable viruses from a publicly available list and released them in airports worldwide,” Esvelt told The Post, “that might be a civilization-level threat.”
The rapid changes in technology have left regulators a step behind, experts say.
That gap became apparent after an NIH-funded researcher named Ron Fouchier in the Netherlands shocked his peers by revealing in 2011 that he had created a mutant strain of a particularly lethal kind of avian flu, H5N1. The resulting pathogen, Fouchier reported, had for the first time spread through respiratory droplets among caged ferrets. The experiment, approved in advance by the NIH, sought to anticipate what might happen if such mutations threaten humans through natural evolution.
Reached by email, Fouchier said his work “filled crucial gaps in knowledge … about what makes an influenza virus transmissible in the air via mammals.” His facilities in Rotterdam, he said, are inspected regularly by Dutch and U.S. government officials, and were “specifically built to work safely and securely with airborne viruses.”
As for what controls are needed globally, Fouchier said: “Authorities should ensure that this type of work can only occur in safe and secure labs, to ensure negligible risk to humans and the environment.”
Fouchier’s work, and several high-profile research mishaps in the United States — including the discovery in 2014 of six vials of virulent smallpox on NIH’s central campus in Bethesda, Md. — alarmed the Obama White House. That fall, officials imposed a moratorium on government-funded experiments with some viruses that would result in a “gain of function,” a change that made the pathogen more lethal, more transmissible or more resistant to drugs or vaccines.
In late 2017, the Trump administration lifted the moratorium and announced new guidelines and an HHS-appointed expert panel to provide oversight. The new system was meant to ensure that U.S.-funded experiments — including those conducted overseas — that could yield more-dangerous viruses would first undergo high-level federal review to assess such projects’ overall risks and potential benefits.
But the policy change applies only to research funded by the HHS and its components, including the NIH. The rules do not encompass experiments that might be backed by the Pentagon, other federal agencies or private companies and institutions.
The 2017 revisions also included an overlooked loophole that exempted experiments from the expert panel’s review unless a lab-created pathogen was “reasonably anticipated’’ to be both “highly transmissible” and “highly virulent.”
In a report in January, the HHS inspector general faulted NIH’s oversight of a project that was launched in China and funded by agency grants from 2014 to 2019 to EcoHealth Alliance, a nonprofit organization based in New York City. According to the report, EcoHealth failed to promptly disclose safety concerns about lab work conducted with coronavirus strains by a subgrantee, the Wuhan Institute of Virology, in the Chinese city where the coronavirus pandemic began. The NIH “did not effectively monitor or take timely action to address EcoHealth’s compliance,” the report said.
In written remarks to the inspector general, EcoHealth’s president, Peter Daszak, disputed that his company had been required to immediately notify NIH of the concerns that the agency later identified. But Daszak also said that EcoHealth had “corrected certain procedures” and aims for “even better compliance” with federal rules.
Asked for comment, EcoHealth reiterated by email the points that Daszak made to the inspector general.
More on Pandemic Risk
Investigations show China is vulnerable to serious lab accidents, exposing problems that allowed deadly pathogens to escape in the past and could well do so again.
Officials at NIH did not contest the conclusions and told the inspector general that corrective actions were underway, including tighter monitoring of foreign subgrantees. Anthony S. Fauci, who was the director of the NIH institute that funded the work in Wuhan, has told Congress that none of those experiments amounted to gain-of-function research. Fauci, 82, retired on Dec. 31.
Le Duc, the infectious-disease expert, and other scientists said the coronavirus pandemic has shown that the federal review standards need to be tightened because even a pathogen that kills at a modest rate can inflict devastation if it is highly transmissible.
In September, the National Science Advisory Board for Biosecurity said the existing definition of pandemic-risk pathogens “should be modified to include potentially highly transmissible pathogens having low or moderate virulence.” That would open more U.S.-funded work to the scrutiny of the HHS panel of experts. In January, the federal board detailed its recommendation in a 29-page report.
Kenneth W. Bernard, a member of the board, told The Post that the proposed change would close “the loophole” and enable stricter scrutiny of high-stakes research. But he said that tighter controls may prompt some virologists to move experiments to less-regulated labs overseas.
“We need to develop incentives for people to put safety and carefulness at the same level as scientific advance,’’ said Bernard, a physician who was a biodefense assistant to President George W. Bush. “The [Biden] administration should move on this quickly.”
The White House expects to address the matter in its planned policy revision, officials said.
‘A legitimate use’
Some bioengineering firms, acutely aware of the potential for harm if their technology is misused, have chosen not to wait for tighter federal rules. They have introduced their own safeguards and oversight systems, voluntarily taking on responsibilities and costs that normally fall to governments.
One of them is the San Francisco company Twist Bioscience.
The 10-year-old firm is among about two dozen globally that synthesize DNA at scale; Twist manufactures artificial genetic sequences to sell to other scientists in labs around the world. Twist’s synthetic DNA is used by researchers to create “designer” bacteria and viruses that can attack cancer cells or clean up oil spills. In theory, it also could be used for malicious purposes, such as tweaking a disease strain to make it more virulent or drug-resistant.
Every day, from inside Twist’s glass office tower near San Francisco International Airport, a machine resembling a 3D printer deposits microscopic strands of genetic code on a silicon wafer as workers in protective gear keep watch. New orders arrive over the internet, and the finished products are sent out the door by courier or mail truck in as little as six days. Concealed within the jumble of coding that makes up a typical order could be the keys to a lifesaving cure — or the biological equivalent of a powerful bomb.
The synthetic-DNA industry is new, and few federal regulations govern it. Asked by The Post about the technology, HHS officials said the department this year is likely to issue “updated guidance’’ for “the gene and genome synthesis enterprise.”
Twist executives, however, say they have already introduced their own safeguards.
In the company’s security department, computers scan each order to see whether the requested DNA matches up with known pathogens, including restricted microbes that cannot legally be acquired without a license. A different team investigates the individuals behind each order. What’s the history and track record of the buyer? Do names and shipping addresses match up? What’s the intended use of the DNA? On a few occasions, a suspicious order has prompted a call to the FBI, company officials said.
“We’re being asked to manufacture this thing, so we have to make sure we truly understand who the ordering party is and whether they have a legitimate use,” said James Diggans, Twist’s head of biosecurity.
The extra steps are costly and time-consuming for a company that has to compete with other synthetic-DNA producers, including in Europe and China. Twist has tried to turn this perceived liability into an asset, marketing itself to customers as a company that sees biosecurity as an essential value that all responsible researchers should share.
Some vendors are less willing to spend the money, particularly in markets overseas, said Emily Leproust, a French-born organic chemist and the company’s co-founder and CEO. Twist has pushed its competitors to abide by the same standards. But with few regulations and no international enforcement, biosecurity remains, for now, a premium feature — an option, for the purveyors of a new science who are sufficiently worried about the risks to take an extra step.
“The majority in the industry are good players, but there a few who don’t participate, and I think it’s wrong,” Leproust said. “Every invention is like a coin, with a side that’s positive and a side that is negative. With dynamite you build a canal. But you can also kill.”
Warrick reported from San Francisco. Alice Crites and Nate Jones in Washington and Emmanuel Martinez in San Diego contributed to this report.